Herbal Supplement Risk Checker
This tool identifies if you're at risk from herbal supplements based on your health conditions or medications. Select all categories that apply to you.
Your Risk Factors
Herbal supplements are everywhere - in pharmacies, grocery stores, and your neighbor’s morning smoothie. They promise energy, better sleep, clearer skin, and even weight loss. But here’s the truth: herbal supplements aren’t harmless candies. For some people, they can be dangerous - even life-threatening.
People on prescription medications
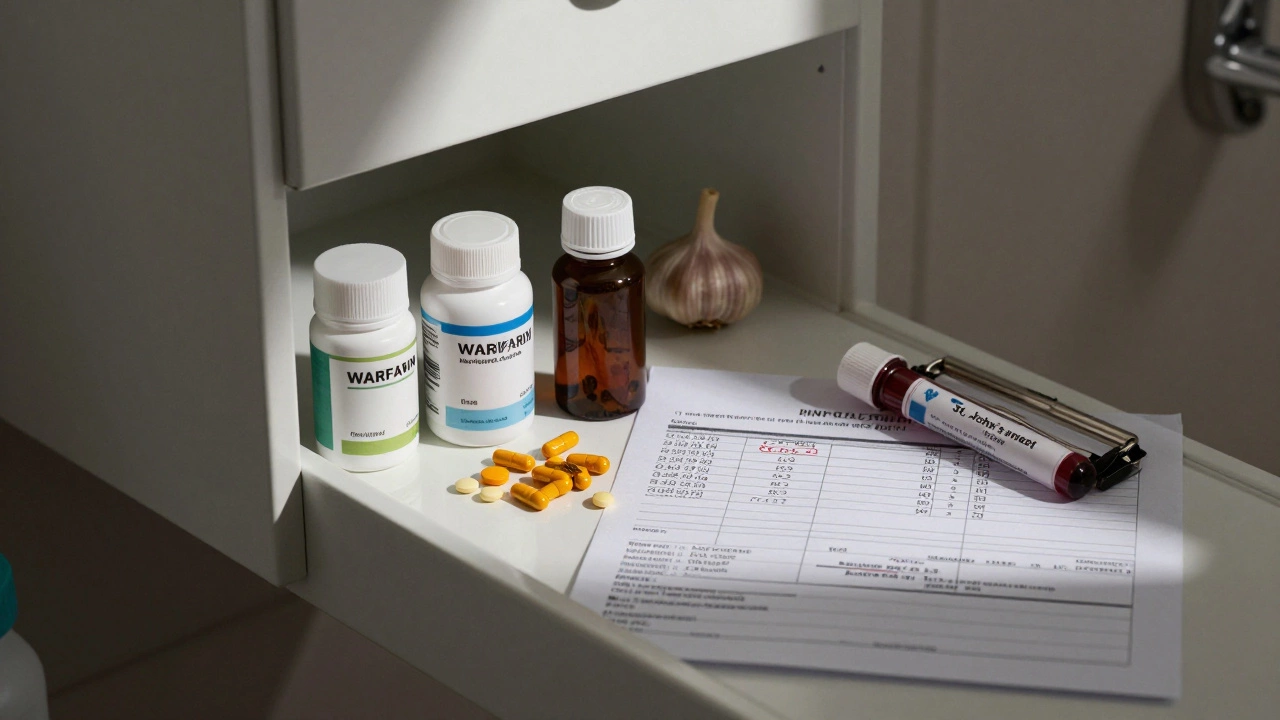
If you take blood thinners like warfarin, don’t assume that turmeric or garlic pills are safe just because they’re "natural." Turmeric contains curcumin, which can thin your blood even more. Garlic supplements do the same. Together, they raise your risk of internal bleeding, especially during surgery or after an injury. A 2023 study in the Journal of Clinical Pharmacology found that over 40% of patients on warfarin who took herbal supplements had dangerous spikes in their INR levels - a measure of blood clotting time. Same goes for statins. St. John’s wort, often used for mild depression, can make cholesterol-lowering drugs like atorvastatin useless. It speeds up how fast your liver breaks them down. You might think your cholesterol is under control, but your bloodwork tells a different story. Antidepressants like SSRIs are another minefield. Supplements like 5-HTP or SAM-e can push serotonin levels too high, leading to serotonin syndrome - a condition that causes confusion, rapid heart rate, fever, and muscle rigidity. It’s rare, but it kills. And no, your pharmacist won’t always catch it. Most herbal products don’t come with warning labels.Pregnant and breastfeeding women
Many women reach for herbal teas or supplements during pregnancy, thinking they’re safer than pills. But chamomile? It can trigger uterine contractions. Black cohosh? Linked to premature labor. Dong quai? It acts like estrogen and may affect fetal development. Even popular herbs like ginger - often recommended for morning sickness - aren’t risk-free. While small amounts (under 1 gram per day) are generally okay, higher doses can interfere with fetal hormone balance. A 2024 review in the British Journal of Obstetrics and Gynaecology found that women who took high-dose herbal supplements in the first trimester had a 27% higher chance of low birth weight. Breastfeeding mothers face similar risks. Herbs like sage and peppermint can reduce milk supply. Others, like licorice root, pass into breast milk and can cause high blood pressure or low potassium in the baby.People with liver or kidney disease
Your liver and kidneys clean out toxins - including herbal compounds. If they’re damaged, those toxins build up. Green tea extract, often sold for weight loss, has been linked to over 100 cases of acute liver failure in the U.S. since 2010. The FDA issued warnings after young, healthy women developed jaundice and liver damage from taking concentrated green tea pills. No one expected a "healthy" supplement to cause this. Kava, used for anxiety, has caused liver failure in Europe and Australia. It’s banned in several countries. Yet it’s still sold online and in health stores. For people with chronic kidney disease, herbs like licorice, horseshoe crab, and aristolochia (found in some traditional remedies) can worsen kidney function. Aristolochia is so toxic it’s been linked to kidney cancer. Even small, long-term doses can be deadly.
People preparing for surgery
If you’re scheduled for surgery, stop all herbal supplements at least two weeks before. This isn’t a suggestion - it’s medical advice. Echinacea, ginkgo, garlic, ginseng, and even ginger can interfere with anesthesia, increase bleeding, or raise blood pressure during surgery. A 2025 survey of 1,200 anesthesiologists in North America found that nearly 60% had encountered patients with unexpected bleeding or heart rhythm issues linked to herbal use. Many patients didn’t even think to mention it. Doctors can’t help you if you don’t tell them. And most herbal labels don’t warn you about surgery risks. That’s on you to know.Children and teenagers
Kids aren’t small adults. Their bodies process herbs differently. Many herbal products are marketed to teens for acne, focus, or weight loss - but they’re not tested for safety in children. Maca root, often promoted for energy and hormones, can trigger early puberty in girls. Ashwagandha, popular for stress, can lower thyroid hormone levels in adolescents, leading to fatigue and weight gain. And melatonin supplements? They’re sold as "natural sleep aids," but they’re unregulated. A 2024 study in the Journal of Pediatric Endocrinology found that over 30% of melatonin products in India contained doses 10 times higher than labeled - and some had traces of serotonin or other drugs. Parents think they’re being safe by choosing "natural." But natural doesn’t mean safe for kids. Always talk to a pediatrician first.
People with autoimmune diseases
If you have lupus, rheumatoid arthritis, multiple sclerosis, or Hashimoto’s thyroiditis, your immune system is already overactive. Some herbal supplements make it worse. Echinacea, astragalus, and elderberry are often sold to "boost immunity." But for autoimmune patients, that’s like pouring gasoline on a fire. A 2023 case series in Arthritis & Rheumatology showed that three patients with lupus had severe flares after taking echinacea for colds. One needed hospitalization. Even turmeric, often praised for its anti-inflammatory effects, can interfere with immune-suppressing drugs like azathioprine. What helps one person can hurt another.What to do instead
You don’t need herbal supplements to be healthy. Food, sleep, movement, and stress management work better - and without the risks. If you’re considering a supplement:- Check with your doctor or pharmacist - don’t assume they’ll know. Bring the bottle.
- Look for third-party testing labels: USP, NSF, or ConsumerLab. These don’t guarantee safety, but they check for contamination and correct dosing.
- Avoid products with "proprietary blends" - you can’t know how much of each herb is in there.
- Stop all supplements at least two weeks before any surgery.
- Report side effects to your country’s health agency. In India, that’s the CDSCO.

Write a comment