Schizophrenia Warning Signs Screener
Assess Potential Warning Signs
This tool helps identify common early indicators of schizophrenia based on clinical research. It does not diagnose or replace professional evaluation.
Next Steps
Early professional evaluation is critical. If this assessment indicates concern:
- • Contact a mental health professional immediately
- • Document specific symptoms and timing
- • Consider a consultation with a psychiatrist or clinical psychologist
When it comes to mental health, Schizophrenia is a chronic brain disorder that typically emerges in early adulthood and can profoundly affect thoughts, emotions, and behavior. Spotting the early warning signs can help families and clinicians intervene before the condition fully develops. Below, we break down the three most common red flags, why they matter, and what steps you can take if you notice them.
Key Takeaways
- The first warning sign often involves subtle changes in perception, like hearing voices that aren’t there.
- Social withdrawal and flat affect are early negative symptoms that can be mistaken for depression.
- Unusual beliefs or magical thinking may signal the onset of delusional thinking.
- Early detection improves treatment outcomes and quality of life.
- Reach out to a qualified mental health professional as soon as you suspect any of these signs.
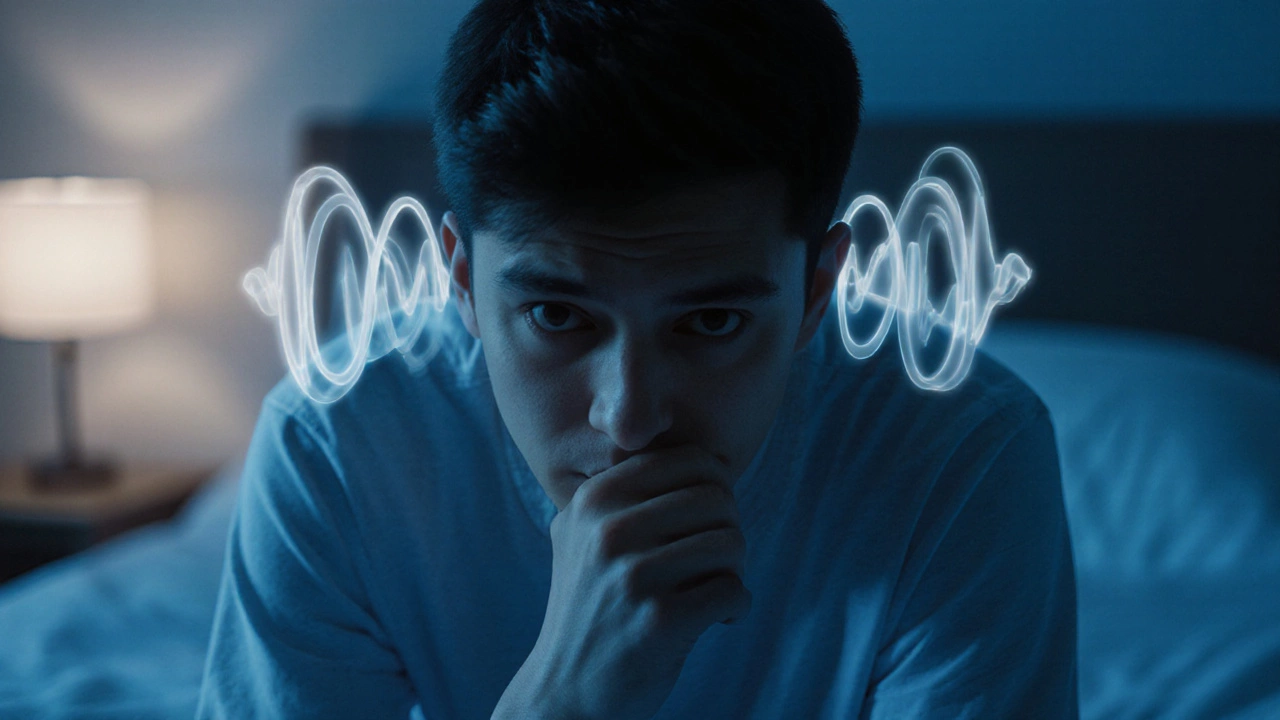
1. Distorted Perception - Hallucinations and Auditory Voices
One of the clearest early indicators is the emergence of hallucination a sensory experience without an external stimulus, most commonly auditory. A person might hear comments, jokes, or commands that no one else hears. These voices can start as occasional whispers and become more frequent over weeks.
Why it matters: Hallucinations are a hallmark of psychosis, the umbrella term for reality‑testing disturbances. If left unchecked, they can evolve into persistent psychotic episodes that impair daily functioning.
What to watch for:
- Talking back to unseen “people.”
- Expressions of fear or agitation without an obvious trigger.
- Sudden changes in sleep patterns due to nighttime voices.
If you notice these cues, encourage the individual to keep a simple diary of when the voices appear. This record helps clinicians differentiate between occasional stress‑related experiences and emerging psychosis.

2. Social Withdrawal and Flattened Affect - The Negative Symptom Cluster
Negative symptoms often sneak in quietly. The most noticeable is a gradual pull‑back from friends, family, and previously enjoyed activities. This withdrawal is accompanied by a flattened affect a reduced expression of emotion, where facial expressions and voice tone become muted. People may seem “numb” or “distant.”
Why it matters: These signs are not just mood‑related; they reflect a deeper disruption in the brain’s reward and motivation pathways. Early negative symptoms predict a more chronic disease course if untreated.
Key observations:
- Loss of interest in hobbies that were once a passion.
- Reduced eye contact and minimal facial expression.
- Speaking in a monotone voice, even when discussing exciting topics.
Action step: Gently prompt the person to share what they’re feeling. Validation without judgment can open the door to professional help.
3. Unusual Beliefs - Early Delusional Thinking
Delusions are firmly held false beliefs that resist logical contradiction. Early signs can appear as “magical thinking” or overly grandiose ideas, such as believing you have secret powers or that everyday events are personal messages.
Why it matters: Delusional thinking shows a breakdown in logical reasoning, a core feature of schizophrenia. When these beliefs intensify, they can lead to risky behaviors or severe paranoia.
Red flags to monitor:
- Claims of being watched, controlled, or having a special mission.
- Insistence on patterns or symbols that others deem random.
- Resistance to accepting evidence that disproves the belief.
Tip: Document specific statements and the context in which they occur. This information is invaluable for a psychiatrist during assessment.
Distinguishing Early Schizophrenia from Common Teen Mood Swings
| Feature | Early Schizophrenia | Typical Mood Swings |
|---|---|---|
| Hallucinations | Frequent, vivid auditory/visual experiences | Rare, usually brief daydreams |
| Social Withdrawal | Progressive disengagement, flat affect | Occasional isolation, still expresses emotions |
| Delusional Beliefs | Fixed false ideas, magical thinking | Exaggerated opinions, but adaptable |
| Functional Decline | Grades dropping, neglect of hygiene | Temporary dips in performance |

Next Steps If You Spot One or More Warning Signs
Early intervention is the game‑changer. Here’s a practical roadmap:
- Talk openly. Approach the person calmly, expressing concern without accusation.
- Gather information. Note dates, frequency, and any triggers associated with the signs.
- Seek a qualified professional. A mental health professional such as a psychiatrist, clinical psychologist, or licensed therapist can conduct a comprehensive assessment using tools like the DSM‑5 criteria.
- Consider a medical review. Some physical conditions (e.g., thyroid issues, substance use) can mimic psychotic symptoms, so a risk factor underlying health or environmental factor that raises likelihood of developing schizophrenia screening may be warranted.
- Explore treatment options. First‑line treatment often involves antipsychotic medication drugs that regulate dopamine pathways to reduce psychotic symptoms combined with psychotherapy, social skills training, and family support.
Remember, treatment works best when started early. Even if symptoms seem mild, professional guidance can prevent escalation.
Supporting a Loved One Through the Early Stages
Family and friends play a critical role. Here are three practical tips:
- Stay educated. Understanding the nature of schizophrenia reduces stigma and improves communication.
- Maintain routine. Consistent sleep, meals, and activity schedules create a stabilizing environment.
- Encourage self‑advocacy. Involve the individual in decisions about treatment to foster empowerment.
Having a supportive network can dramatically improve adherence to medication and therapy, leading to better long‑term outcomes.
Frequently Asked Questions
Can teenagers experience these warning signs, or are they only for adults?
Yes, early onset schizophrenia often appears in late teens to early twenties. The signs look similar but may be confused with typical adolescent mood swings, which is why careful observation and professional evaluation are essential.
How long do these warning signs usually last before full‑blown schizophrenia develops?
The prodromal phase can last from several months up to a few years. Early detection and treatment during this window can delay or even prevent the transition to chronic psychosis.
Are there any non‑medication approaches that help with early symptoms?
Cognitive‑behavioral therapy (CBT) for psychosis, social skills training, and structured family interventions have shown benefits in reducing symptom severity and improving daily functioning.
What lifestyle factors can increase the risk of developing schizophrenia?
Key risk factors include a family history of schizophrenia, early cannabis use, high‑stress environments, and prenatal complications. Reducing substance use and managing stress can lower the likelihood of onset.
Is it possible to recover completely if caught early?
While schizophrenia is considered a chronic condition, many individuals achieve substantial remission with early, consistent treatment. Quality of life can be high when symptoms are well‑managed.

Write a comment