Cancer Risk Assessment Tool
Assess Your Cancer Risk
Not all cancers are the same. Some grow slowly, respond well to treatment, and have high survival rates. Others? They strike fast, hide deep, and fight back harder than most doctors expect. If you’ve ever wondered which cancers are the most dangerous, you’re not alone. The truth isn’t about fear-it’s about awareness. Knowing which cancers are the toughest to beat can help you spot warning signs early, ask the right questions, and push for faster action.
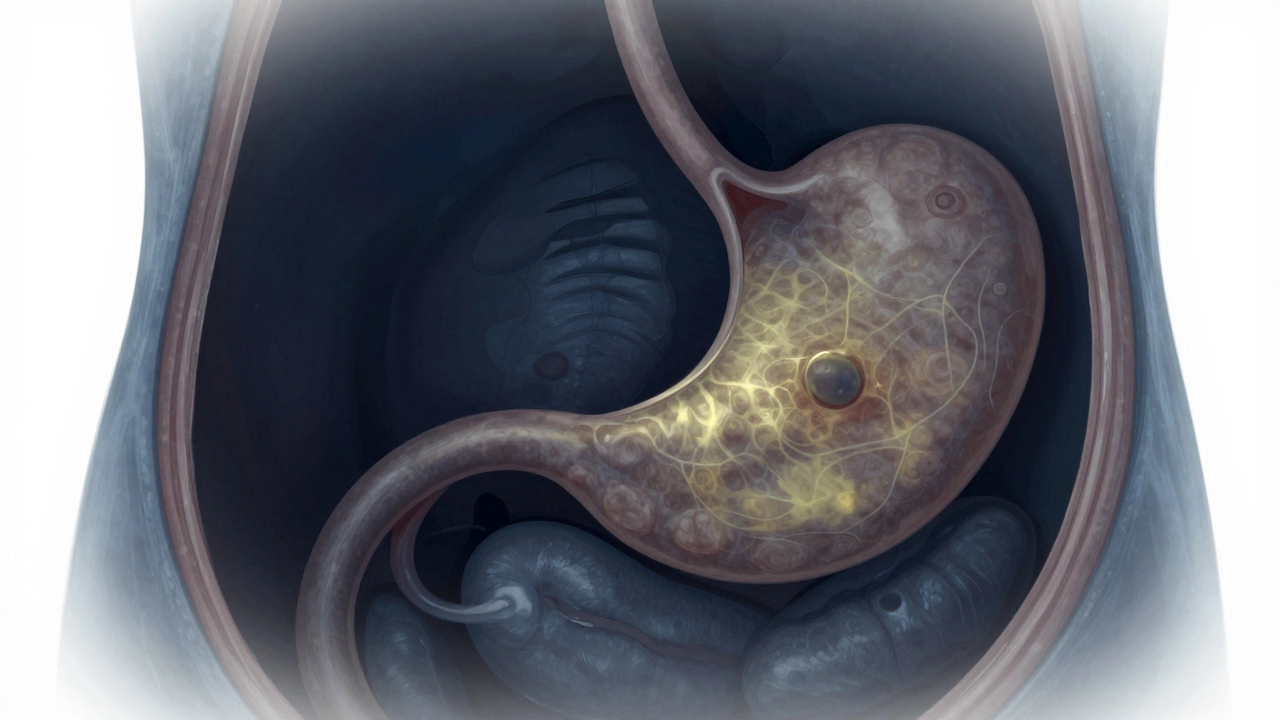
Pancreatic Cancer: The Silent Killer
Pancreatic cancer doesn’t shout. It whispers. By the time symptoms show up-like unexplained weight loss, yellowing skin, or new-onset diabetes-it’s often too late. Only about 10% of people diagnosed with pancreatic cancer survive five years. That’s the lowest survival rate of any major cancer.
Why? The pancreas sits deep inside the abdomen, behind the stomach. Tumors grow without pushing on anything noticeable until they’ve spread to nearby organs or blood vessels. There’s no routine screening test like a mammogram or colonoscopy. Doctors can’t catch it early unless someone is already at high risk-like those with inherited gene mutations or chronic pancreatitis.
Even when surgery is possible, the recurrence rate is high. Chemotherapy and radiation help, but they rarely cure. New treatments like immunotherapy are being tested, but progress is slow. In 2025, pancreatic cancer is still the third leading cause of cancer-related death in the U.S. and rising fast in India, where diets high in processed foods and low in fiber are becoming more common.
Lung Cancer: Still the #1 Cancer Killer
Lung cancer kills more people every year than breast, prostate, and colorectal cancers combined. Even though smoking rates have dropped in many countries, lung cancer hasn’t. Why? Because it’s not just smokers. Around 20% of lung cancer deaths happen in people who never smoked. Secondhand smoke, air pollution, radon gas, and even cooking fumes in poorly ventilated kitchens play a role-especially in places like rural India where chulhas are still common.
Small cell lung cancer (SCLC) spreads fast. Non-small cell lung cancer (NSCLC) is more common but still deadly if caught late. Symptoms like a persistent cough, chest pain, or coughing up blood often get dismissed as a cold or bronchitis. By the time imaging shows a tumor, it’s often stage III or IV.
But here’s the twist: survival has improved for some. If caught early-through low-dose CT scans for high-risk people-five-year survival jumps to 60%. The problem? Fewer than 5% of eligible people in India get screened. Targeted therapies and immunotherapy have helped some patients live years longer, but only if the cancer has specific genetic markers. Without testing, those treatments don’t even get a chance.

Ovarian Cancer: The Whispering Disease
Ovarian cancer is called the "silent killer" for a reason. Most women don’t feel anything until the cancer has spread beyond the ovaries. By then, it’s often in the abdomen, wrapped around the intestines or liver. The five-year survival rate? Just 31% for advanced cases.
There’s no reliable screening test. Pap smears don’t catch it. CA-125 blood tests are too vague-they rise for many reasons, not just cancer. Ultrasounds can miss small tumors. Symptoms? Bloating, feeling full fast, pelvic pain, frequent urination. These are easy to brush off as digestive issues or stress. In India, where women often delay doctor visits due to stigma or lack of access, the delay can be months-or years.
Genetics matter. Women with BRCA1 or BRCA2 mutations have up to a 44% lifetime risk. But most don’t know they carry the gene. Even when diagnosed, treatment is brutal: surgery to remove ovaries, uterus, and lymph nodes, followed by harsh chemotherapy. Recurrence is common. New drugs like PARP inhibitors help some women stay in remission longer, but they’re expensive and not widely available outside major cities.
Why These Three Stand Out
What makes pancreatic, lung, and ovarian cancers so deadly isn’t just how fast they grow-it’s how well they hide. They don’t cause obvious pain early on. They don’t show up on basic tests. And when they’re found, they’ve often already spread.
Compare that to breast or skin cancer. A lump you can feel. A mole that changes. These are visible. Easy to catch. Early detection saves lives. But with these three cancers, early detection is the exception, not the rule.
Another factor: funding. Research dollars for pancreatic and ovarian cancer lag behind breast or prostate cancer. Public awareness campaigns are quieter. There’s no pink ribbon for pancreatic cancer. No bold campaigns for ovarian cancer awareness. That silence costs lives.

What You Can Do
You can’t control your genes. But you can control your awareness.
- If you have a family history of ovarian, breast, or pancreatic cancer, ask about genetic testing.
- If you’re a long-term smoker or live in a high-pollution area, talk to your doctor about a low-dose CT scan for lung cancer.
- If you’re over 50 and suddenly lose weight without trying, get your pancreas checked-not just your stomach.
- If you feel bloated for more than two weeks, with no clear reason, don’t wait. See a gynecologist.
These cancers don’t care if you’re young, old, healthy, or active. They don’t wait for perfect timing. But your body gives signals-if you know what to listen for.
Hope Is Growing
It’s not all grim. New blood tests for early pancreatic cancer are in clinical trials. Liquid biopsies for ovarian cancer are showing promise. Lung cancer treatments are becoming more personalized, with drugs targeting specific mutations like EGFR and ALK.
In Bangalore, hospitals like Apollo and Manipal are now offering multi-gene panels for hereditary cancer risk. More clinics are starting to screen high-risk patients. Awareness is slowly rising.
Survival rates aren’t fixed. They change with research, policy, and public pressure. The more people talk about these cancers, the more doctors listen. The more we push for screening, the earlier we catch them.
Don’t wait for a symptom to become unbearable. Don’t assume it’s just aging or stress. If something feels off-persist. Ask for tests. Push for answers. You might just save your life-or someone else’s.
What makes pancreatic cancer so hard to detect?
Pancreatic cancer is hard to detect because the pancreas is hidden deep in the abdomen, and early tumors don’t cause obvious symptoms. By the time pain, weight loss, or jaundice appear, the cancer has often spread. There’s no standard screening test for the general population, and blood tests like CA-125 aren’t reliable for this cancer.
Can you survive lung cancer if you never smoked?
Yes, but it’s still dangerous. About 20% of lung cancer deaths occur in people who never smoked. Causes include secondhand smoke, air pollution, radon gas, and genetic factors. Survival depends on early detection. Low-dose CT scans can catch tumors before they spread, especially in high-risk groups like older adults with long-term exposure to pollutants.
Is ovarian cancer only a concern for older women?
No. While risk increases after menopause, ovarian cancer can strike younger women too-especially those with BRCA gene mutations. Symptoms like bloating, pelvic pain, and feeling full quickly can appear at any age. Many young women dismiss these signs as PMS or digestive issues, delaying diagnosis. Genetic testing and awareness are critical for all women with a family history.
Are there screening tests for these cancers?
Only for lung cancer-low-dose CT scans are recommended for high-risk individuals, like long-term smokers over 50. For pancreatic and ovarian cancer, no routine screening exists for the general public. Genetic testing for BRCA mutations can help identify high-risk individuals for ovarian and pancreatic cancer. Always discuss your personal risk with a doctor.
Can lifestyle changes reduce the risk of these cancers?
For lung cancer, quitting smoking is the single biggest step. For pancreatic cancer, avoiding obesity, heavy alcohol use, and processed meats helps. For ovarian cancer, birth control pills and breastfeeding can lower risk. Regular exercise and eating more vegetables may also help. But genetics play a big role-so lifestyle alone isn’t enough. Awareness and early testing matter more.

Write a comment