
If your knee feels like a rusty hinge every morning and crunches with every step, you might wonder, “How bad does it need to get before I’m looking at knee replacement?” You’re not alone—this question comes up a lot in doctor’s offices. The truth? There’s no magic number, but there are patterns and red flags you can spot before it gets unbearable.
Think about what you can’t do anymore. Struggling to climb stairs, limping at the grocery store, delaying outings because your knee acts up—these are everyday warning signs. Sometimes the pain creeps in so slowly you don’t realize how much you’ve changed your routine until someone points it out. If painkillers barely help and you find yourself skipping things you used to love, your knee is telling you something important.
- Spotting the Signs: How Bad Is Bad?
- Daily Life: When Knee Pain Takes Over
- What Doctors Look For
- When Other Treatments Don’t Work
- Getting Ready for Knee Replacement
Spotting the Signs: How Bad Is Bad?
First off, you don’t need to be doubled over in agony every day to consider knee replacement. It’s not just about pain. Doctors look at a handful of tell-tale signs. You want to catch them before things get worse.
The main red flag? Stubborn, deep knee pain that sticks around for months, especially when you’re moving. Some people feel it throbbing at night or even when just sitting. This isn’t garden-variety muscle soreness from yard work. We’re talking pain that messes with your sleep or makes you dread every step.
You might also notice the knee is always stiff. If it takes you longer to get up from a chair, or you’ve developed a limp to “protect” your bad side, this matters. Swelling that doesn’t quit—sometimes for weeks or months—can mean it’s not just a passing thing.
Dr. Emily Laskowski from the Mayo Clinic puts it simply:
“When knee pain starts interfering with your daily activities—walking, climbing stairs, even getting up from a chair—that’s a strong signal your knee isn’t coping and you might need to look at replacement.”
To help spot these warning signs, here’s a quick list of questions that doctors use:
- Are you using pain meds almost every day, but they barely help?
- Do you avoid seeing friends or running errands because of your knee pain?
- Is your knee always swollen or buckling under you?
- Have your hobbies taken a back seat—like gardening, walking, or sports—because of knee trouble?
- Has your doctor said your osteoarthritis looks really bad on X-rays?
Statistically, about 90% of people who end up getting a knee replacement were getting less than 60% of normal knee function before surgery. That’s a huge drop-off, and most put off the decision for years.
| Sign | What it Means |
|---|---|
| Constant pain | Joint damage or osteoarthritis |
| Severe stiffness | Knee mobility is going down |
| Recurring swelling | Inflammation that isn’t improving |
| Instability | Knee gives way unexpectedly |
| Failed treatments | Pills, injections, or therapy no longer work |
Bottom line: It’s not about being “tough.” If your knee health is shutting down your life, that’s when most doctors say it’s time to talk about your next steps.
Daily Life: When Knee Pain Takes Over
When your knee pain hits the point where even simple stuff feels like a challenge, it’s time to pay attention. People usually notice trouble with things like standing up from a chair, walking more than a few blocks, or getting in and out of the car. If you’re using the handrail just to make it up a single step, your knee is more than just “acting up.”
Most folks with real knee pain due to osteoarthritis (that’s the most common reason for knee replacement) start making small but important life changes without even realizing it. Maybe you stop walking your dog, let grocery shopping slide, or start asking for help a lot more than usual. Over time, these little changes add up and make a big difference in your quality of life.
Doctors sometimes use specific questions to track how much your knee health affects your daily life. Here are a few common problems people report:
- Your knee hurts even when you’re sitting or lying down.
- Pain and stiffness first thing in the morning or after sitting for a while (called 'start-up pain').
- Swelling that never really seems to go away.
- Trouble sleeping because of knee pain.
- Difficulty putting on socks and shoes.
Here’s something most people never hear: Studies from big groups, like the American Academy of Orthopaedic Surgeons, show that people who wait too long for knee replacement often recover more slowly after surgery. Simply put, living with pain for months or years can actually make things harder after the fix. You don’t get a medal for toughing it out until walking is almost impossible.
| Everyday Task | % Reporting Difficulty (severe knee arthritis) |
|---|---|
| Standing up from a chair | 65% |
| Going up/down stairs | 80% |
| Walking more than 100 meters | 70% |
| Sleeping through the night | 45% |
So if your day starts and ends with working around your knee pain, you’re not alone—and you don’t have to just put up with it forever. Recognizing when your daily life is taking a hit is a sign it might be time to talk seriously about solutions, including knee replacement.
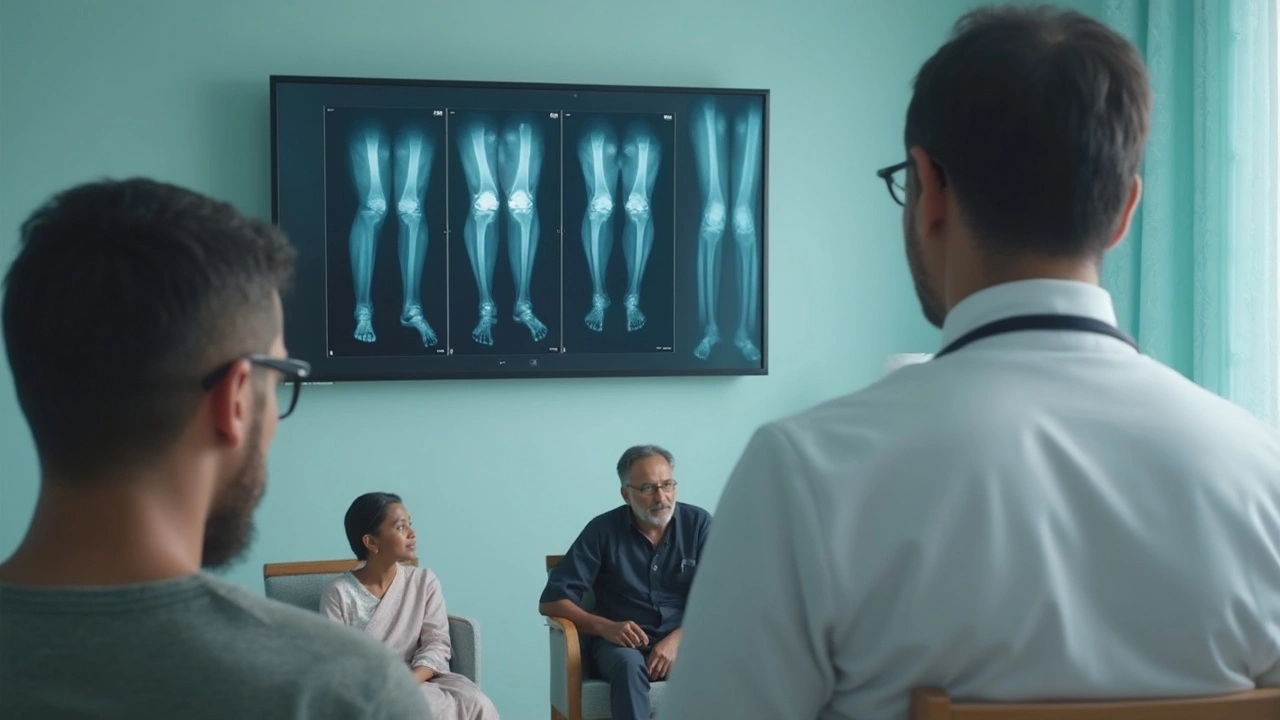
What Doctors Look For
When it comes to knee replacement, doctors don’t just look at your X-rays and say, “That’s it, you need surgery.” They go through a whole checklist to understand how messed up your knee health really is. The decision between toughing it out and signing up for knee replacement is never random.
First, your doctor asks a lot of questions about your daily life. Are you able to walk a block, go up the stairs, or get in and out of a chair without grabbing the furniture? Is pain waking you up at night, or keeping you from sleeping?
Here’s what your doctor actually looks for:
- Pain level: If you’re dealing with pain most days, and it doesn’t get better with rest or painkillers, that’s a clue you may need joint surgery.
- Mobility struggles: If your range of motion has tanked—like you can’t bend or straighten your knee—it’s not a good sign. Trouble with daily activities carries a lot of weight.
- X-ray results: They’ll want to see the joint space in your knee. If there’s little to no space left and the bones are rubbing, it usually means severe osteoarthritis.
- Swelling and stiffness: If your knee is stiff every morning or stays swollen, doctors take that seriously.
- Other treatments failed: They’ll check if you’ve tried exercise, physical therapy, shots, or medications. If nothing helps, knee replacement moves up on the list.
Doctors also rate pain and function on a scale. A common method is the Oxford Knee Score—a simple questionnaire that checks how your knee feels during basic activities. Lower scores mean your life is more limited by knee trouble.
| Factor | Sign of Needing Knee Replacement |
|---|---|
| Pain (scale 1-10) | 7 or higher most days |
| Range of motion | Limited bend or unable to straighten knee |
| X-ray | Bone rubbing on bone |
| Failed non-surgical treatments | Yes |
Doctors really want to be sure you’ve tried everything else first. If you’re ticking most of these boxes, your knee may be waving a giant “Help me!” sign. But the final call always comes down to your own quality of life and what you’re willing to live with.
When Other Treatments Don’t Work
Most people don’t jump straight to knee replacement. Doctors usually bring out their full toolbox before talking about surgery. This means months—sometimes years—of trying things like physical therapy, pain meds, injections, braces, and all kinds of stretches. If you’re still stuck with knee pain after all that? That’s a big red flag.
Here’s what usually comes before knee surgery:
- Painkillers and anti-inflammatories: Over-the-counter stuff like ibuprofen or prescription meds. If these only last a few hours or don’t touch the pain, it’s a sign your joint damage is serious.
- Physical therapy: Targeted exercises to strengthen muscles and improve range of motion. Sometimes, this works wonders. Other times, it barely scratches the surface.
- Steroid injections: These shots can give quick relief, but if they don’t help—or they wear off in days instead of months—it’s a clue your knee’s too far gone.
- Hyaluronic acid injections: Think of this as adding lubricant. Some people swear by them, but science shows benefits are usually small and short-lived, especially if you’re already in a lot of pain.
- Weight loss and activity adjustments: Losing just ten pounds can take a serious load off the knees. But if you do that and you’re still miserable, it’s a sign the joint can’t keep up anymore.
Doctors usually call it “end-stage osteoarthritis” when all these options flop. By then, the cartilage is worn down, bone rubs on bone, and nothing in the usual toolkit makes much difference. A 2023 study found most people who go for knee replacement have lived with moderate to severe pain for over a year, despite trying at least two or three treatments.
If you're checking off all these boxes and still walking around with a limp or waking up every night, it’s probably time to have that tough conversation about knee replacement. The goal isn’t just to cut pain—it’s to actually get your life back.

Getting Ready for Knee Replacement
So, you and your doctor have decided a knee replacement is on the cards. It feels like a big step, but getting prepared makes a huge difference in how things go. There’s a real checklist that people swear by—let’s break it down without the boring fluff.
First, your doctor will likely order blood tests, a chest X-ray, and sometimes an EKG to make sure your body can handle surgery. If you have other health problems like diabetes or heart issues, get those as stable as you can. Surgeons don’t just want your knee fixed—they want the rest of you in good shape, too.
Next up, your home setup matters more than you might guess. After joint surgery, you’ll probably use a walker or crutches for a bit. Rearrange furniture so you have clear paths. Move essentials like snacks, chargers, and toiletries to waist height. Some folks rent a toilet seat riser or a shower chair, and trust me, these aren’t just for the elderly—they make life way easier for everyone who’s just had their knee replaced.
While it’s not glamorous, most hospitals ask if you’ve got help lined up for those first couple of weeks. If you live alone, see if a friend or family member can stick around or check in on you. Many people try to cook and freeze meals ahead of time. You’ll be surprised how much little things, like ready meals, help you focus on recovery and physical therapy.
If you’re curious about the numbers, check this table out. It breaks down the timeline most people experience with knee replacement:
| Stage | What Usually Happens |
|---|---|
| 2-4 Weeks Before | Pre-op checkups, tests, stop certain meds if needed |
| 1 Week Before | Prep home, arrange transportation and help, shop for recovery supplies |
| Day of Surgery | Arrive fasting, surgery itself lasts about 1-2 hours |
| First Few Days After | Hospital stay (sometimes same-day discharge), start light physical therapy |
| First 2 Weeks After | More physical therapy, staples out if used, home recovery |
Don’t forget to talk to your surgeon about the exact plan—they all have their routines and preferences. And if you have questions, write them down. There’s a lot to remember when nerves kick in.
Prepping for a knee replacement is a bit like prepping for a marathon, but the finish line is pain-free movement. Take every step seriously, but don’t stress—you’re far from the first to walk this path. A solid plan now means smoother days ahead.

Write a comment