
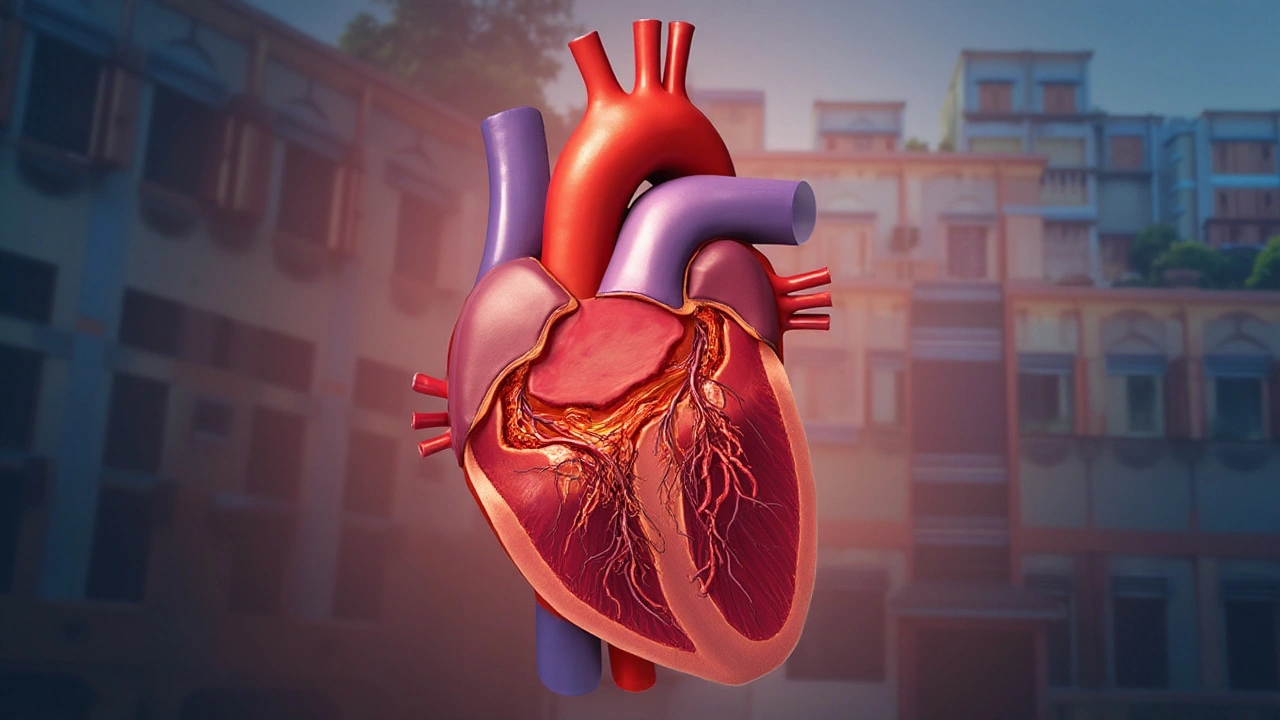
Heart surgery can sound intimidating, especially when you're facing a procedure yourself or for a loved one. Yet, understanding what these surgeries entail can provide reassurance and clarity, making them seem less daunting. Various types of heart surgeries are designed to tackle specific heart-related issues, ensuring the best possible outcomes for patients.
From the commonly performed Coronary Artery Bypass Grafting (CABG) to intricate procedures involving valve repair, each type of surgery has its own approach and benefits. With advancements in medical technology, some surgeries are now minimally invasive, allowing for quicker recovery times and shorter hospital stays.
Knowing what to expect can be empowering. Whether it's learning about the intricacies of the procedures or the steps involved in recovery, this knowledge helps patients make well-informed choices about their heart health.
- Introduction to Heart Surgery
- Coronary Artery Bypass Grafting (CABG)
- Heart Valve Repair and Replacement
- Pacemaker and Implantable Devices
- Minimally Invasive Heart Surgery
- Post-Surgical Care and Recovery
Introduction to Heart Surgery
Heart surgery, a remarkable feat of modern medical science, serves as a lifeline for countless individuals facing critical heart health issues. It's a specialized field that has witnessed tremendous advancements over the decades, thanks to the relentless efforts of cardiac surgeons and researchers. At its core, heart surgery involves procedures aimed at correcting problems with the heart—whether they're congenital, a result of lifestyle factors, or due to the wear and tear that accompanies aging. These surgeries can range from coronary artery bypass grafting to heart transplants, each addressing specific cardiac concerns. While the thought of undergoing heart surgery can evoke anxiety, understanding the need, process, and success rates can demystify these life-saving procedures.
The development of heart surgery as a branch of medicine took off in the 20th century when techniques to operate on a still or beating heart were first introduced. One milestone in heart surgery was the first successful open-heart procedure performed by Dr. John Gibbon, who used a heart-lung machine to take over the heart's functions temporarily. Since then, technology and techniques have evolved dramatically. Today, minimally invasive techniques allow surgeons to perform complex operations through small incisions, reducing recovery time and potential complications. Renowned surgeon Dr. Christiaan Barnard, who performed the world's first human heart transplant, once said, "Surgery is always a partnership, a pact between the patient and the surgeon striving for the best outcome."
Deciding to undergo heart surgery is deeply personal, influenced by a myriad of factors including the patient’s health, the type of surgery required, and the expected outcomes. It's not just about fixing a heart—it’s about restoring quality of life, offering the patient the ability to return to activities they love, and sometimes, it's about survival. Statistics show significant improvements in survival rates; for instance, five-year survival rates post-coronary artery bypass grafting are more than 90% when performed in time. Such numbers are a testament to the effectiveness of these procedures in enhancing longevity and quality of life.
An integral aspect of heart surgery is the preparation and post-operative care. Preparation involves thorough diagnostic tests to ensure the patient's suitability for surgery, as well as discussions about potential risks and benefits. Recovery, on the other hand, is a collaborative effort between the healthcare providers and the patient, focusing on rehabilitation, lifestyle changes, and regular monitoring. The journey from diagnosis to recovery can be long and challenging, but many find it rewarding after experiencing the renewed vigor in their day-to-day lives.
Coronary Artery Bypass Grafting (CABG)
When we talk about coronary artery bypass grafting, or CABG as it is commonly known, we're looking at one of the most frequently performed heart surgeries in the world. This procedure is specifically aimed at improving blood flow to the heart. Unfortunately, when coronary arteries become blocked or narrowed, due to plaque buildup, people might experience severe chest pain, known as angina, or even suffer a heart attack. CABG tackles this issue head-on by using a healthy artery or vein from another part of the body to create a new path around the blocked artery.
The grafted artery or vein helps redirect the blood around the obstructed or narrowed artery, essentially ‘bypassing’ the problematic section. The procedure is usually recommended for patients suffering from severe coronary artery disease, especially when medications or other treatments haven’t worked, or if multiple coronary arteries are blocked. Astonishingly, CABG has a long history, with the first successful surgery performed in 1960, and has since saved countless lives. According to the National Heart, Lung, and Blood Institute, thousands of CABG operations are done each year in the United States alone, testifying to its critical role in combating heart disease.
Due to the intricate nature of the surgery, CABG typically requires open heart surgery where the chest is opened to access the heart. Doctors will often advise patients on how to prepare beforehand, which may include guidelines on medication, diet, and physical activities. Because every patient's case is unique, personalized advice is essential. After discussing with experienced surgeons, many patients find comfort in knowing that the overall success rate of CABG is quite high.
"CABG remains a cornerstone treatment for heart disease, significantly improving both lifespan and quality of life," says Dr. John Mack, renowned cardiologist at the American Heart Care Institute.
While undergoing CABG surgery, patients are usually under general anesthesia, and the surgical team relies on a heart-lung machine to keep blood circulating while the heart is temporarily stopped. This allows surgeons the precise control needed to create the bypass. In some cases, however, surgeons opt for an off-pump or beating-heart surgery, eliminating the need for the heart-lung machine. This technique can be an advantage in certain patient populations, reducing some risks associated with the traditional method.
Post-surgery, attention shifts to recovery. Patients spend time in the intensive care unit (ICU) where their vital signs are closely monitored. With advancements in medical care, most find themselves gradually regaining strength, supported by medications that help control pain and prevent complications. The recovery period is crucial, encouraging lifestyle changes such as adopting a heart-healthy diet and regular exercise routine. An intriguing fact is that many patients also join cardiac rehabilitation programs which have been shown to enhance recovery outcomes significantly.
The economic impact of CABG is noteworthy too, as it reflects the costs associated with advanced healthcare solutions. The operation itself, along with ongoing management, contributes to substantial expenses; however, the overall benefit in terms of improved quality of life and prevention of costly complications like heart attacks is invaluable. As researchers continue to innovate and improve surgical techniques, the future of CABG looks promising, offering hope to patients facing the challenges of heart disease.
Heart Valve Repair and Replacement
The heart is a marvel of a machine, meticulously designed to keep us alive and thriving. It relies heavily on its four valves—the aortic, mitral, pulmonary, and tricuspid—to regulate blood flow. However, when these valves malfunction due to stenosis or regurgitation, heart valve repair and replacement surgeries become necessary interventions. These procedures aim to restore proper heart function and alleviate symptoms such as fatigue and shortness of breath, significantly improving a patient's quality of life. Heart surgery performing doctors often have to assess whether repair or replacement is the best course of action depending on the damage and the cause of valve disease. Repair is typically preferred whenever possible, as it retains the patient's own tissues, avoiding the complications of prosthetic devices.
Heart valve repair involves techniques like valve leaflet reshaping, ring annuloplasty, and de-calcifying the valve tissue. Ring annuloplasty, for instance, focuses on reinforcing the valve with a ring to ensure closure, especially in cases of valve dilation. On the contrary, valve replacement is needed when the valve is too damaged to repair. This involves substituting the faulty valve with either a mechanical or biological one. Mechanical valves have remarkable durability but require lifelong blood-thinning medication to prevent clots. Biological valves, often made from porcine or bovine tissue, offer a more natural function but may need replacement after 10-15 years. As technology progresses, we are witnessing the rise of transcatheter valve replacement systems, which are less invasive and offer hope for patients unable to withstand traditional surgery.
"The decision between repair versus replacement is incredibly nuanced,” says Dr. Christine Albert, Chair of Cardiology at Cedars-Sinai Heart Institute. “We're continually improving our techniques and devices to not only extend life but enhance its quality."Heart health professionals consider individual patient needs, the nature of the valve damage, and the risks involved in each option carefully. According to the American Heart Association, valve disease affects roughly 2.5% of the population, with risk increasing with age. Given the complexity and variety of types of heart surgery procedures available, a detailed discussion with a cardiologist is paramount to decide the best course. Many times these interventions turn into life-saving procedures, steering patients back to routines they cherish. When considering any cardiac procedure, understanding the nature of the condition and potential treatment options aids in alleviating anxiety and fostering proactive health management.
Pacemaker and Implantable Devices
A pacemaker is a small device that's placed in the chest or abdomen to help control abnormal heart rhythms. It uses electrical pulses to prompt the heart to beat at a normal rate. These devices can be temporary, like those used during an operation or after a heart attack, or they can be permanent. Permanent pacemakers may have one or two wires that guide the electrical impulses either to the heart's upper chambers, the lower chambers, or to both.
The role of a pacemaker can be life-changing for individuals with conditions like bradycardia, where the heart beats too slowly, or heart block, which disrupts the signals passing from the heart's upper to lower chambers. Focusing on heart health, these devices ensure a regular heartbeat, effectively mitigating symptoms like fatigue, dizziness, and fainting. According to the American Heart Association, over one million people worldwide are fitted with a pacemaker annually, showcasing their critical role in cardiac care.
Complementary to pacemakers are other implantable devices such as implantable cardioverter-defibrillators (ICDs). While pacemakers regulate slow rhythms, ICDs prevent sudden death by correcting dangerously fast heart rhythms that could lead to cardiac arrest. An ICD is more than just a defibrillator; it serves as a pacing mechanism too, addressing slow heartbeats by delivering low-energy electrical pulses. Moving from pacemakers to broader implantable devices allows patients to consider other tailored medical innovations available to support heart function.
"The evolution of cardiac devices like pacemakers has revolutionized the way we approach heart disease management, offering patients reliable and life-enhancing solutions," states Dr. Michael Jones, a renowned cardiologist.
Implantation of these devices, though common, isn't without risk, necessitating careful consideration and discussion with a healthcare provider. Surgical risks include infection and swelling, while device-based risks might involve lead dislodgement or equipment malfunction. Post-surgery, patients typically require follow-up visits to ensure device functionality and battery life, typically lasting 5-15 years depending on device usage.
Advancements and Innovations
Technological advancements continue to refine these cardiac surgery solutions. Some newer devices are leadless, reducing risks related to the leads used in traditional pacemakers. These wireless versions are implanted directly in the heart, allowing for minimally invasive procedures. Moreover, advanced ICDs now include remote monitoring features, enabling healthcare providers to adjust settings or diagnose issues from afar. This technological curve not only simplifies device management but also enhances patient experience significantly.
- Patients should avoid electromagnetic fields that could interfere with device functioning, such as strong magnets or metal detectors.
- Regular follow-ups are vital for checking the device's battery life and functionality.
- Individuals with pacemakers should inform all healthcare providers of their device, especially in situations requiring medical imaging like MRIs.
Understanding the array of pacemakers and implantable devices available allows patients to make informed decisions. Recognizing that these devices are more than just medical equipment — they're lifelines, offering peace of mind and enabling individuals to continue thriving, despite heart health challenges.

Minimally Invasive Heart Surgery
Minimally invasive heart surgery is revolutionizing the way we approach cardiac procedures today. Unlike traditional open-heart surgery, which involves a large incision and splitting the breastbone, minimally invasive techniques use smaller incisions that often lead to faster recovery times, less pain, and reduced risk of infection. This approach has become increasingly popular as technology has advanced, providing equally effective results for certain types of heart conditions. For patients with severe blockages or faulty heart valves, minimally invasive options can offer a lifeline with fewer complications and quicker return to normal activities. While not every patient is a candidate for these techniques, those who are can expect a different experience from the more conventional approach.
One of the most common forms of minimally invasive heart surgery is robotic-assisted surgery. This technique allows surgeons to perform complex heart procedures using a console that guides robotic arms. The precision offered by robotic systems enables more accurate surgery, benefitting intricate repairs like those needed for heart valve procedures. Another minimally invasive option is thoracoscopic surgery, which employs a small camera inserted into the chest, offering a clear view of the heart on a monitor. This procedure eliminates the need for significant incisions, which can translate to a shorter hospital stay and faster healing times.
When considering minimally invasive approaches, it's crucial to understand that surgical outcomes and recovery experiences can vary. According to a study published in The Journal of Thoracic and Cardiovascular Surgery, minimally invasive aortic valve replacement showed a comparable success rate to traditional methods but boasted a significantly reduced recovery period.
Dr. Alice Johnson, a renowned cardiac surgeon, states, "Minimally invasive procedures are not just about smaller incisions; they represent a paradigm shift in how we approach cardiac surgery by significantly enhancing patient comfort and recovery times."As cardiac technology continues to advance, the scope of these procedures is expected to broaden, potentially encompassing more complex heart surgeries in the future.
Deciding on a surgical option can involve weighing many factors, including the specific heart condition, the patient's overall health, and personal preferences. It's essential to consult with a specialized cardiac surgeon to determine the best course of action. They can provide detailed information about the potential risks and benefits associated with minimally invasive heart surgery, ensuring patients make informed decisions about their heart health.
In some cases, keyhole techniques might not be suitable, and traditional surgery remains the best option. However, for those eligible, the advantages are compelling. A holistic approach considering long-term outcomes is always recommended. The success of the surgery doesn't merely depend on the procedure itself but also on diligent post-operative care, monitoring, and lifestyle adjustments, emphasizing the need for a comprehensive treatment plan.
Post-Surgical Care and Recovery
After the successful completion of heart surgery, the recovery journey begins, which is a vital part of the patient's overall treatment. This phase involves both hospital-based and home-based care, requiring a collaborative effort among healthcare professionals and family members. Initially, patients spend time in the intensive care unit (ICU) under close monitoring, which helps in managing any immediate post-operative concerns such as bleeding or arrhythmias. During this period, heart function and vital signs are continuously checked to ensure stability and address any complications swiftly.
Once out of the ICU, a patient's recovery continues in the regular hospital ward where they begin to engage in simple physical movements and breathing exercises. These activities aim to improve circulation, prevent blood clots, and enhance lung function, essential for a swift recovery. Around this time, doctors also carefully adjust medication dosages to manage pain and prevent infection, directly contributing to the healing process. Dietary changes may also be initiated to support cardiac health, with a focus on low-sodium and nutritious meals.
Discharge from the hospital marks the beginning of home-based recovery, which often involves a structured cardiac rehabilitation program. These programs are tailored to help patients regain physical strength and confidence in their activities of daily living. Rehabilitation includes supervised exercise routines, along with educational sessions focusing on lifestyle changes necessary to maintain heart health, such as smoking cessation and stress management. Patients are encouraged to slowly increase their activity levels as advised by their healthcare providers, ensuring a balance between rest and exertion.
Pacemaker implantation or other devices require specialized care instructions, such as wound care and activity restrictions, to prevent complications. It's vital for patients to attend regular follow-up appointments to monitor their progress and adjust their treatment plans as necessary. The involvement of family members and caregivers makes a significant difference, providing emotional support and practical assistance when needed.
During this time, adhering to prescribed medications remains crucial. These might include anticoagulants, beta-blockers, or statins, each playing a role in safeguarding heart health. Patients must be vigilant about experiencing any new symptoms, like increased fatigue or irregular heartbeat, and report these promptly to their healthcare team. Emotional well-being is also significant; it's not uncommon to feel a range of emotions such as anxiety or depression following cardiac surgery. Seeking support through counseling or community groups can be beneficial.
According to the American Heart Association, "Cardiac rehabilitation does not change your past, but it can help you improve your heart’s future." This encapsulates the essence of post-surgical recovery — a reinvestment in one's health to foster a stronger heart and a healthier lifestyle.
Recovery timelines can vary widely among patients, influenced by factors such as the type of surgery undergone, pre-existing health conditions, and individual patient resilience. Patience and perseverance are equally as important as medical interventions, as gradual improvements lead to long-term benefits. Properly managing this phase of care enhances not only the success of the surgery itself but also the patient's quality of life going forward.

Write a comment