
Dental Implant Candidacy Calculator
This calculator helps you assess your candidacy for dental implants based on key medical factors. Answer the questions below to receive a personalized report.
Answer the questions above to see your dental implant candidacy.
Wondering if you’ve missed the window for dental implants? It’s a common worry, especially as the years stack up or health issues creep in. The truth is, there isn’t a single age cut‑off; instead, a mix of bone health, gum condition, and overall medical status decides whether an implant will hold up. This guide walks you through the key factors that signal you might be too late, how to assess your own situation, and what backup plans exist if implants aren’t the right fit.
What Exactly Are Dental Implants?
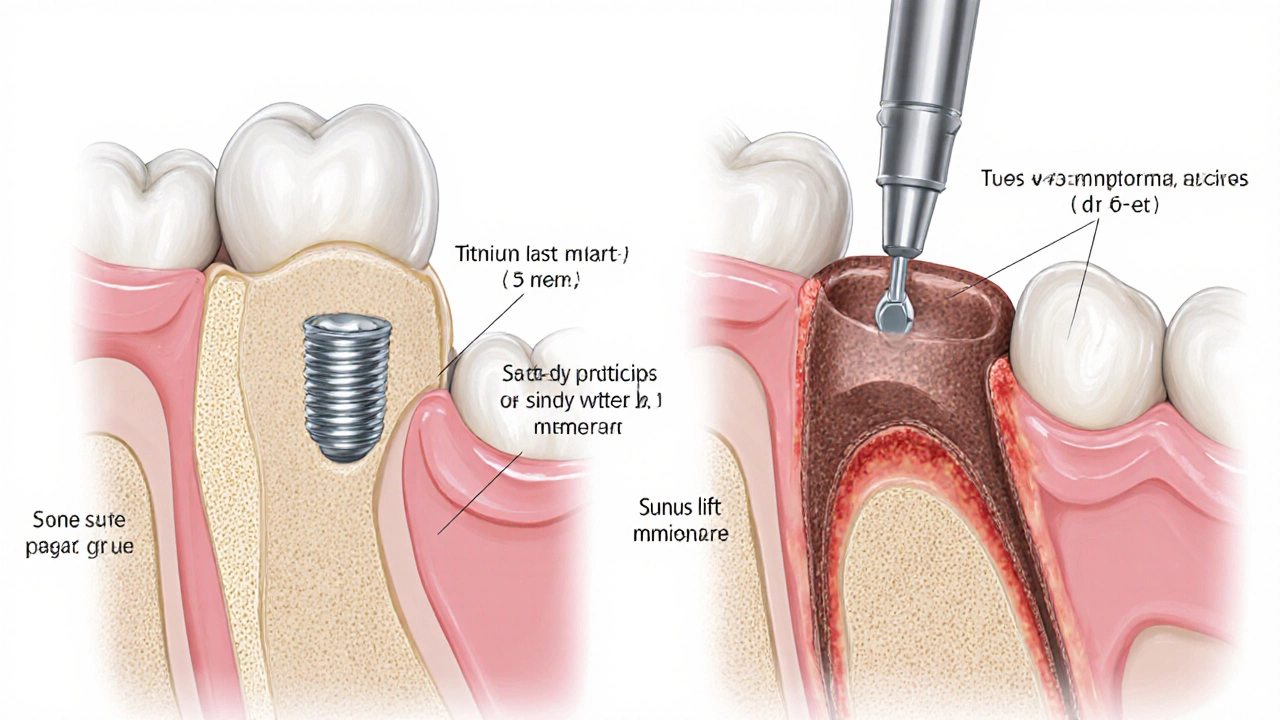
Dental implants are titanium posts surgically placed into the jawbone to act as artificial tooth roots. They fuse with bone through a process called osseointegration, providing a sturdy base for crowns, bridges, or dentures. The goal is to restore chewing function and aesthetics with something that feels and works like a natural tooth.
Key Factors That Influence Implant Suitability
Instead of counting birthdays, clinicians look at a checklist of health markers. If you meet most of the criteria, you’re likely a good candidate-even in your 70s.
- Bone volume and density: Sufficient jawbone is essential for the implant to anchor securely.
- Gum health: Active gum disease (periodontitis) can undermine implant stability.
- Systemic conditions: Uncontrolled diabetes, osteoporosis, or certain medications may slow healing.
- Lifestyle habits: Smoking, heavy alcohol use, or poor oral hygiene increase failure risk.
- Overall health status: Patients must be fit for minor oral surgery under local anesthesia.
When Bone Loss Becomes a Deal‑Breaker
If you’ve lost a tooth for years, the surrounding bone can begin to resorb-think of it like a hollow where the tooth used to be. When the vertical height drops below about 5mm or the width under 6mm, standard implants may not have enough purchase.
Bone grafting is a surgical procedure that adds bone material (autograft, allograft, or synthetic) to rebuild the missing volume. While grafts dramatically improve success rates, they also add treatment time (often 4-6 months for healing) and cost. If you’re not willing or able to undergo grafting, implants might not be realistic.
Gum Disease - The Silent Saboteur
Periodontitis is chronic inflammation of the gums that erodes both soft tissue and underlying bone. Even mild cases can jeopardize an implant’s integration. Dentists will usually treat the infection first-deep cleanings, antibiotics, and sometimes surgical pocket reduction-before considering implants.
If you notice bleeding gums, persistent bad breath, or loose teeth, those are red flags that you should address before any implant talk.
Age‑Related Conditions: Osteoporosis and Sinus Proximity
Osteoporosis reduces bone density throughout the skeleton, including the jaw. In severe cases, the bone may be too porous to hold an implant without supplemental procedures.
For upper‑back teeth, the implant tip can encroach on the sinus cavity. When the sinus floor is too low, a sinus lift procedure elevates the sinus membrane and adds bone graft material to create safe space for the implant. This is a common solution, but not everyone wants the added surgery.
Systemic Health Checks: Diabetes and Medications
Well‑controlled type2 diabetes (HbA1c<7%) generally doesn’t stop implants, but uncontrolled blood sugar can impair healing and raise infection risk. Certain meds-like bisphosphonates for osteoporosis-have been linked to rare cases of jaw osteonecrosis after invasive dental work.
Always share your full medical history with the oral surgeon; they’ll decide if a waiting period or medication adjustment is needed.
Decision Matrix: Ideal, Challenging, and Contra‑indicated Scenarios
| Criteria | Ideal | Challenging | Contra‑indicated |
|---|---|---|---|
| Bone Height (mm) | >10 | 5‑10 (requires graft) | <5 (multiple grafts or not feasible) |
| Bone Density | Dense (D1‑D2) | Moderate (D3) | Very low (D4) or osteoporotic |
| Gum Health | Healthy, no bleeding | Mild periodontitis (treated) | Active severe periodontitis |
| Systemic Condition | Stable, controlled chronic disease | Uncontrolled diabetes, recent steroids | Bisphosphonate therapy, radiation to jaw |
| Lifestyle | Non‑smoker or quit >6months | Light smoker (≤10 cig/day) | Heavy smoker (>10 cig/day) |
This matrix helps you self‑screen before the first appointment. If you land in the “challenging” column, don’t panic-most issues are solvable with pre‑treatment steps.
How to Get a Professional Verdict
- Schedule a comprehensive oral exam. The dentist will check for decay, gum disease, and overall oral hygiene.
- Get radiographic imaging. A Cone‑Beam CT (CBCT) scan offers a 3‑D view of bone volume, sinus proximity, and nerve canals.
- Discuss medical history. Bring a list of current meds, chronic conditions, and lifestyle habits.
- Ask about adjunct procedures. If bone or sinus issues appear, learn the timeline and success rates for grafts or lifts.
- Review the treatment plan and cost. Some clinics bundle grafts, implants, and crowns into a single quote; others itemize each step.
Make sure the clinician you choose is a board‑certified oral and maxillofacial surgeon or a periodontist with extensive implant experience.
Alternatives When Implants Aren’t Viable
If the suitability checklist lands you in the “contra‑indicated” zone, there are still ways to restore function and smile confidence.
- Removable dentures: Modern acrylic or flexible dentures can be stable, especially with adhesive.
- Fixed dental bridges: Use adjacent teeth as anchors; requires prepping healthy teeth.
- All‑on‑4 or All‑on‑6: A hybrid approach where a few strategically placed implants support a full arch-often works even with moderate bone loss.
- Mini‑implants: Smaller diameter posts that can be placed in thinner bone; less invasive and quicker healing.
Each option has pros and cons regarding longevity, comfort, and cost. A thorough discussion with your dentist will pinpoint the best fit for your lifestyle.
Tips to Boost Implant Success If You’re on the Edge
- Quit smoking at least six weeks before surgery; it improves blood flow and bone healing.
- Maintain a balanced diet rich in calcium, vitaminD, and protein to support bone health.
- Control chronic illnesses-regularly monitor blood sugar if diabetic.
- Practice impeccable oral hygiene: floss daily, use antiseptic mouthwash, and keep quarterly cleanings.
- Consider a short‑term probiotic protocol to reduce post‑op infection risk (studies show a 30% drop in complications).
Even if you start with borderline bone, these habits can tip the odds in your favor.
Frequently Asked Questions
At what age do dental implants become unsafe?
There isn’t a strict age limit. Implants can succeed well into the 70s and 80s if bone quality, gum health, and systemic conditions are favorable. The key is a personalized medical assessment, not a birthday.
Can I get implants if I have mild osteoporosis?
Mild osteoporosis often isn’t a blocker. Your dentist may order a bone density scan and, if needed, recommend a bone graft or a shorter implant design to accommodate thinner bone.
How long does a sinus lift add to the treatment timeline?
A sinus lift typically requires 4-6months of healing before the implant can be placed. Some clinicians use a staged approach, placing the implant at the same time as the lift, but this depends on bone quality.
Will smoking disqualify me from getting implants?
Heavy smoking significantly raises failure risk, so most surgeons ask patients to stop for at least six weeks before and after surgery. Light smokers may still be eligible but will be counseled on quitting.
Are there non‑surgical alternatives if I can’t get implants?
Yes. Removable dentures, traditional bridges, and mini‑implant‑supported overdentures are effective options that avoid major bone surgery.

Write a comment